Intra-Aortic Balloon Pump: The Latest Updates
Introduction
The Intra-Aortic Balloon Pump (IABP) has been a cornerstone of mechanical circulatory support for decades, providing temporary assistance to the failing heart by improving coronary perfusion and reducing afterload. While newer devices like Impella® and ECMO have entered the scene, IABP still holds a vital role in specific clinical scenarios.
For advanced practice registered nurses (APRNs) and other cardiac care providers, staying current on IABP indications, evidence, and evolving technology is essential—not only for optimal patient care but also for meeting continuing education goals through specialized courses like those offered by APRN WORLD.
A Quick Refresher on IABP Function
The IABP is inserted via the femoral or axillary artery, with its balloon positioned in the descending thoracic aorta. It inflates during diastole to increase coronary artery perfusion and deflates just before systole to reduce left ventricular workload.
Latest Evidence on IABP Efficacy
Declining Use in Cardiogenic Shock
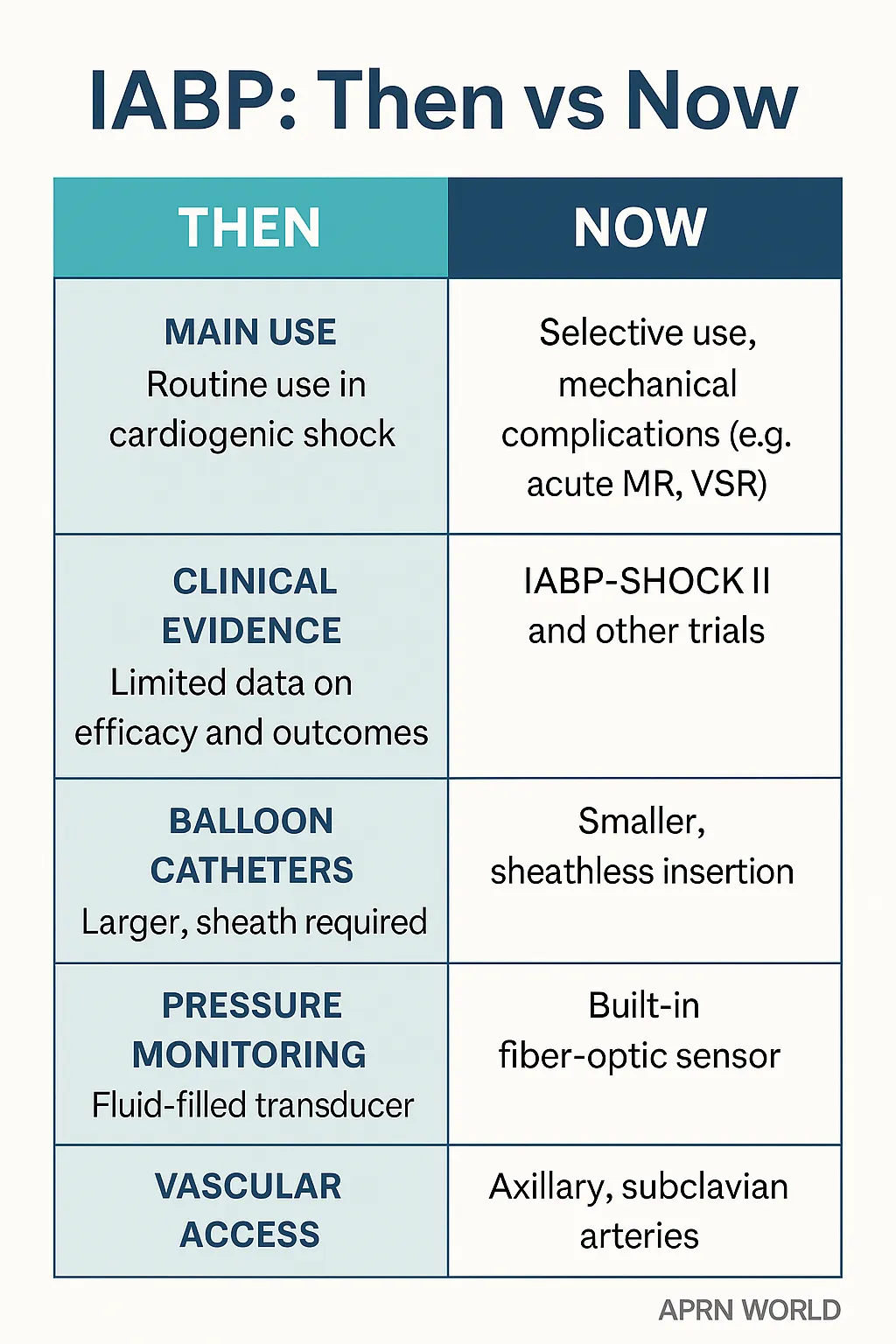
The landmark IABP-SHOCK II trial and subsequent studies showed no significant mortality benefit in acute myocardial infarction with cardiogenic shock, leading to more selective use. Updated guidelines from the ESC and AHA now reserve IABP for specific hemodynamic profiles or as a bridge to more advanced support.
Emerging Roles
Preoperative Stabilization: High-risk CABG patients may benefit from preoperative IABP to optimize perfusion.
Mechanical Complications of MI: Still recommended in cases such as acute severe mitral regurgitation or ventricular septal rupture while awaiting surgery.
Bridge to Decision: Short-term support while determining long-term device or transplant eligibility.
Technology Improvements in IABP Devices
Smaller Catheters and Sheathless Insertion
Newer catheters reduce vascular complications and enable placement in patients with smaller arteries. Sheathless insertion also lowers bleeding risk.
Fiber-Optic Technology
Built-in fiber-optic sensors allow real-time arterial pressure monitoring without the need for external transducers—improving accuracy and reducing setup time.
Alternative Access Routes
Axillary and subclavian artery insertion techniques now allow patient ambulation, crucial for those requiring longer support without being bedridden.
Integration into Multimodal Support Strategies
In modern cardiac care, IABP is often part of a tiered mechanical support plan, used in conjunction with inotropes, Impella®, or ECMO—especially in centers with heart team protocols.
Educational Implications for APRNs
For APRNs, staying proficient in IABP management, troubleshooting, and patient selection is essential. Continuing education should cover:
Hemodynamic principles of counterpulsation
Timing waveform interpretation
Weaning strategies
Complication recognition and prevention
APRN WORLD’s Cardiology CEU modules include hands-on and case-based training for these skills, ensuring providers can translate guidelines into bedside excellence.
Conclusion
While the IABP is no longer the first-line therapy for all cardiogenic shock cases, it remains a valuable tool in specific, high-risk cardiac scenarios. Technological upgrades have improved safety, ease of use, and patient mobility. For APRNs, mastering IABP care means understanding its evolving role in evidence-based, patient-centered cardiovascular management.
Enhance your expertise in cardiac assist devices—enroll in APRN WORLD’s Advanced Cardiovascular Support CEU Course to gain practical, evidence-based skills for IABP management and beyond.










