Immediate Post-Operative Care in Cardiac Surgery: Best Practices
Introduction
The moments following a cardiac surgery are some of the most critical in a patient’s recovery journey. Whether the procedure is coronary artery bypass grafting (CABG), valve replacement, or congenital heart defect repair, the immediate post-operative phase demands vigilant monitoring, prompt intervention, and evidence-based decision-making.
For Registered Nurses (APRNs), mastering post-op care protocols is essential—not only to optimize patient outcomes but also to fulfill continuing education requirements through specialized training like APRN WORLD’s Cardiac Surgery CE courses.
Goals of Immediate Post-Operative Care
Stabilize hemodynamic status
Maintain adequate oxygenation and ventilation
Prevent early complications (bleeding, arrhythmias, low cardiac output)
Support organ function and tissue perfusion
Provide optimal pain control for recovery
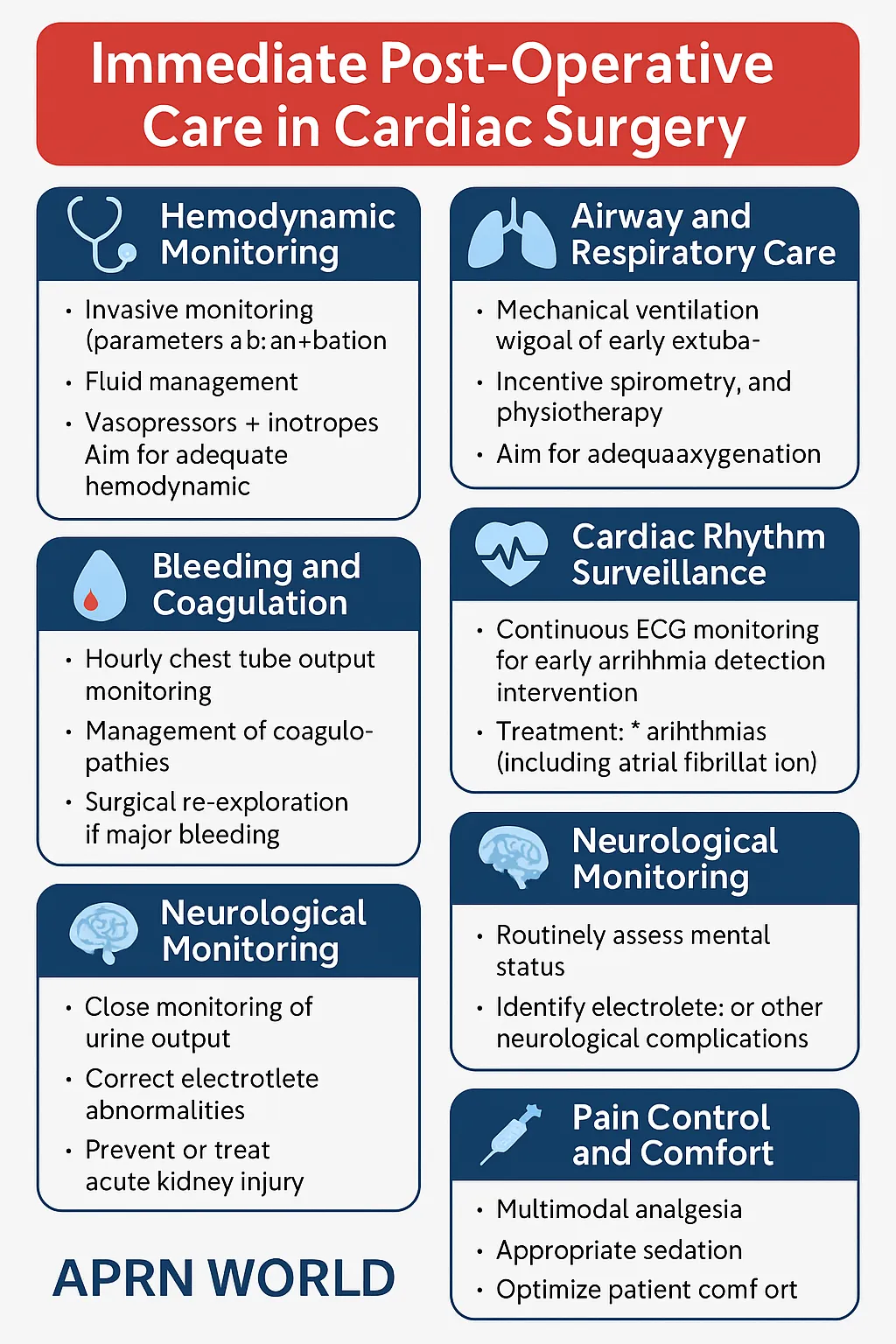
Hemodynamic Monitoring and Stabilization
Invasive Monitoring
Arterial lines for continuous blood pressure monitoring
Central venous pressure (CVP) and pulmonary artery catheters to assess fluid status and cardiac output
Continuous ECG to detect arrhythmias early
Fluid and Vasopressor Management
Balance between avoiding fluid overload and maintaining adequate preload
Titrate vasopressors/inotropes based on hemodynamic targets and organ perfusion
Airway and Respiratory Care
Most patients arrive in the ICU intubated and mechanically ventilated
Early extubation (within 6–12 hours if stable) improves outcomes
Incentive spirometry and chest physiotherapy post-extubation prevent atelectasis and pneumonia
Bleeding and Coagulation Management
Hourly chest tube output monitoring for the first 6–12 hours
Prompt surgical re-exploration if bleeding exceeds thresholds (e.g., >200 mL/hr for 2–3 hours)
Correct coagulopathies with targeted blood product administration
Cardiac Rhythm Surveillance
Common Early Arrhythmias
Atrial fibrillation—occurs in up to 40% of post-CABG patients
Ventricular arrhythmias—often due to electrolyte imbalances or ischemia
Temporary epicardial pacing may be necessary for bradyarrhythmias or AV block
Neurological Monitoring
Early neuro checks to assess for post-op stroke or hypoperfusion injury
Continuous sedation assessment to balance comfort with ability to evaluate mental status
Renal Function and Electrolyte Balance
Strict input/output monitoring to detect acute kidney injury early
Frequent potassium and magnesium checks—critical for arrhythmia prevention
Pain Control and Comfort Measures
Multimodal analgesia (opioids + acetaminophen + regional techniques) to reduce opioid requirements
Adequate pain control improves respiratory effort, mobility, and healing
Infection Prevention
Strict sterile technique for invasive lines and chest tube sites
Early removal of unnecessary catheters and drains
Prophylactic antibiotics per surgical protocol
RN Role in the Post-Op Cardiac ICU
As primary bedside providers, RNs integrate continuous monitoring, early intervention, patient/family education, and care coordination. Their advanced assessment skills and evidence-based decision-making significantly impact recovery trajectories.
APRN WORLD CE courses cover:
Hemodynamic waveform interpretation
Mechanical ventilation weaning strategies
Post-op arrhythmia management
Evidence-based protocols for bleeding and infection control
Conclusion
The first 24 hours after cardiac surgery can determine the success of the entire operation. Through precise monitoring, rapid intervention, and interdisciplinary teamwork, RNs play a central role in ensuring patients transition safely from surgery to recovery.
Call-to-Action (CTA)
Advance your cardiac critical care skills—enroll in APRN WORLD’s Immediate Post-Operative Care in Cardiac Surgery CEU Course to master the latest evidence-based protocols for high-acuity patients.










